
By Dr. Mercola
There is a staggering amount of misinformation on diabetes, a growing epidemic that afflicts more than 29 million people in the United States today. The sad truth is this: it could be your very OWN physician perpetuating this misinformation
Most diabetics find themselves in a black hole of helplessness, clueless about how to reverse their condition. The bigger concern is that more than half of those with type 2 diabetes are NOT even aware they have diabetes — and 90 percent of those who have a condition known as prediabetes aren’t aware of their circumstances, either.
Diabetes: Symptoms of an Epidemic
 |
||||||
 |
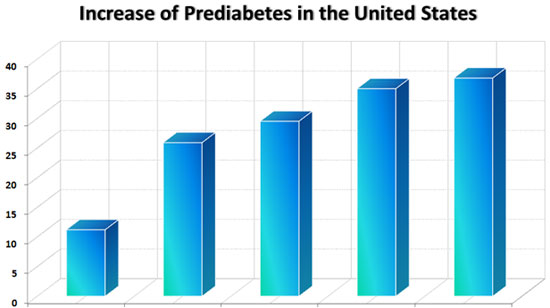
1979 to 1980 (11.2%) | 2003 to 2006 (25.9%) | 2005 to 2006 (29.5%) | 2007 to 2009 (25%) | 2020 (36.8%) |  |
The latest diabetes statistics1 echo an increase in diabetes cases, both diagnosed and undiagnosed. By some estimates, diabetes has increased more than 700 percent in the last 50 years!
At least 29 million Americans are diagnosed with type 2 diabetes, and another 86 million are prediabetic.
What’s hidden behind this medical smokescreen is that type 2 diabetes is completely preventable. The cure lies in a true understanding of the underlying cause (which is impaired insulin and leptin sensitivity) and implementing simple, inexpensive lifestyle adjustments that spell phenomenal benefits to your health.
Type 1 Diabetes and Insulin Dependence
Also known as diabetes mellitus, type 1 diabetes is a chronic health condition traditionally characterized by elevated levels of glucose in your blood, often simply called “high blood sugar.”
Type 1 diabetes – dubbed “juvenile onset diabetes” – is the relatively uncommon type, affecting only about 1 in 250 Americans. Occurring in individuals younger than age 20, it has no known cure.
What’s most concerning about juvenile diabetes is that, these numbers have been going up steadily right along with type 2 diabetes: for non-Hispanic white youths ages 10 to 14, the rates have risen 24 percent in the past few decades.
But even more significant is that for black children, they’ve gone up 200 percent! And, according to recent studies, these numbers are predicted to double by 2020 for all youth.2
In type 1 diabetes, your own immune system ravages the insulin-producing cells of your pancreas. The result is a loss of the hormone insulin. Type 1 diabetics need to be supplemented with insulin for the rest of their lives as failure to do so will rapidly result in death. At the current time, other than a pancreas transplant there is no known cure for type 1 diabetes.
Type 2 Diabetes: Virtually 100 Percent Curable
The far more common form of diabetes is type 2, which affects 90 to 95 percent of diabetics. In this type, your body produces insulin but is unable to recognize and use it properly. It is considered an advanced stage of insulin resistance. Insulin resistance allows glucose in your body to increase and cause a host of complications.
The signs of diabetes may all be there, but the often-overlooked fact is that type 2 diabetes is completely preventable and nearly 100 percent curable. Some of the signs that you may be diabetic are:
| Excessive thirst | Extreme hunger (even after eating) |
| Nausea and possible vomiting | Unusual gain weight or loss |
| Increased fatigue | Irritability |
| Blurred vision | Slow healing of wounds |
| Frequent infections (skin, urinary, and vaginal) | Numbness or tingling in hands and/or feet |
How They Got It All Wrong About Diabetes
Diabetes is NOT a disease of blood sugar, but rather a disorder of insulin and leptin signaling that evolves over a long period of time, moving first into a prediabetes state, and then to full-blown diabetes if left unchecked. One reason mainstream medicine largely fails in treating diabetes with anything other than insulin shots or pills – and sometimes even worsens it – is because it refuses to act on this underlying cause. Insulin sensitivity is key in this matter.
The purpose of your pancreas is to produce the hormone insulin and secrete it into your bloodstream, thereby regulating your glucose at the levels your body needs to live.
The function of insulin, then, is to act as a source of energy for your cells. In other words you NEED insulin to live, and normally your pancreas does its job of providing your body with just the right amount. But certain risk factors and other circumstances may put your pancreas at risk of not functioning properly.
Risk Factors for Type 2 Diabetes (Source: The National Diabetes Education Program)
Age 45 or older Overweight or obese Family history of diabetes Hypertension Physical inactivity Depression History of gestational diabetes Atherosclerotic cardiovascular disease HDL-C levels under 35mg/dL Fasting triglycerides over 250 mg/dL Treatment with atypical antipsychotics, glucocorticoids Obstructive sleep apnea and chronic sleep deprivation Certain health conditions associated with insulin resistance Member of high-risk population (African American, Hispanic/Latino, Native, or Asian American)
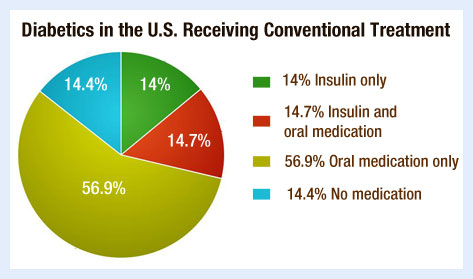
Chances are, if you have one or more of these risk factors, or if your blood glucose levels are elevated, you’ll be checked for diabetes and put on insulin, either in pill form or by injection — and sometimes both.
Your doctor will say that the purpose of taking these shots or pills is to lower your blood sugar. He may even explain to you that this is necessary because insulin regulation plays such as an integral role in your health and longevity. He might add that elevated glucose levels not only are symptoms of diabetes, but also of heart disease, peripheral vascular disease, stroke, high blood pressure, cancer, and obesity. And of course, your doctor would be correct in all of that.
But would he or she go beyond that explanation to tell you what part leptin plays in this process, or that when your body develops a resistance to leptin, you’re on your way to diabetes, if you’re not already there?
Probably not.
Diabetes and Leptin and Insulin Resistance
Leptin is a hormone produced in your fat cells. One of its primary roles is to regulate your appetite and body weight. It tells your brain when to eat, how much to eat, and when to stop eating, which is why it’s called the “satiety hormone.” It also tells your brain what to do with the energy it has.
Not very long ago it was determined that mice without any leptin became very obese. Similarly, in humans, when you become leptin resistant, that mimics leptin deficiency and it becomes easy for you to rapidly gain weight.
You can thank the discovery of leptin and its role in the body to Jeffrey M. Friedman and Douglas Coleman, two researchers who discovered this hormone in 1994. Interestingly, Friedman named leptin after the Greek word "leptos", which means “thin,” after he discovered that mice injected with synthetic leptin became more active and lost weight.
But when Friedman also found that obese people have very high levels of leptin in their blood, he decided that something else must be going on. And that “something” was that obesity can cause a resistance to leptin — in other words, the signaling pathway for leptin becomes skewed in obese people, causing the body to over-produce leptin just as it does glucose when you are insulin-resistant.
Friedman and Coleman also discovered that leptin is responsible for the accuracy of insulin signaling and for your insulin resistance.
Thus, the primary role of insulin is NOT to lower your blood sugar, but to store the extra energy (glycogen, a starch) for present and future consumption. Its ability to lower your blood sugar is merely a “side effect” of this energy storage process. Ultimately, what this means is that diabetes is both a disease of insulin and of a malfunction in leptin signaling.
And that’s why “treating” diabetes by merely concentrating on lowering blood sugar can be a dangerous approach. It simply does not address the actual issue of metabolic miscommunication that’s going on in every cell of your body when your leptin and insulin levels are disrupted and stop working together the way they should.
Taking insulin may even spell greater trouble for some type 2 diabetes patients, as it will worsen their leptin and insulin resistance over time. The only known way to reestablish proper leptin (and insulin) signaling is through your diet. And I promise, your diet can have a more profound influence on your health than any known drug or modality of medical treatment.
Fructose: A Driving Force Behind the Diabetes and Obesity Epidemic
An expert in leptin resistance and its role in making you diabetic is Dr. Richard Johnson, head of Nephrology at the University of Colorado. Dr. Johnson has been an important contributor to my articles on sugar, obesity, and diabetes. 3 His book, The Fat Switch, shatters many of our age-old myths about diet and weight loss.
Dr. Johnson reviews this fascinating topic in the video below, in which he carefully explains how consuming fructose activates a powerful biological switch that causes us to gain weight. Metabolically, this is a highly beneficial capability that allows many species, including humans, to survive times of food scarcity.
Unfortunately, if you live in a developed country today where food is abundant and easily available, this fat switch has lost its biological advantage, and instead of helping many people live longer, it is actually working to their disadvantage and killing them prematurely.
You might be interested to know that “death by sugar” is not at all an exaggeration. The overwhelming amount of fructose in the standard American diet is a major factor in the rise of diabetes rates in this country. While glucose is designed to be used by your body for energy (regular sugar is 50 percent glucose), fructose breaks down into a variety of toxins that can devastate your health.
The Fat Switch also documents many of the adverse effects of fructose such as:
- Elevates uric acid, which may lead to inflammation and a host of other diseases that include hypertension, kidney disease, and fatty liver
- Leads to insulin resistance, an underlying factor in type 2 diabetes, heart diseases, and many cancers
- Tricks your body into gaining weight by deceiving your metabolism. Fructose doesn’t appropriately stimulate insulin, which, as a result, fails to suppress ghrelin ("hunger hormone") and to stimulate leptin ("satiety hormone")
- Rapidly leads to metabolic syndrome, or weight gain and abdominal obesity (beer belly), decreased HDL, increased LDL, elevated triglycerides, elevated blood sugar, and high blood pressure
- Metabolizes like ethanol, causing toxic effects like non-alcoholic fatty liver diseases (NAFLD)
Government Corn Subsidies Make the Problem Even Worse
Lawmakers whose campaigns are underwritten by agribusinesses use billions of taxpayer dollars to subsidize the commodities that are the key ingredients of unhealthy food such as corn, soybeans, and wheat. This manufactured price inequality helps junk food — which is made largely of corn, soybean, and wheat products — undersell nutritious fresh, whole (and REAL) food.
Corn and soybeans are at the top of the list of subsidy gluttons, and are scheduled to total $3.37 billion in just one year alone: fiscal 2017 — a 38 percent increase over what they collected in 2014.4
And if the future is reflective of the past, the subsidies will only be going up, although the Congressional Budget Office (CBO) is saying they will go down in three or four years (something I wouldn’t hold my breath for).
There's a common belief that healthy, fresh, whole, and organically-grown food is inherently more expensive, and thus can only be for the wealthy. But in fact, healthy food could easily be more affordable for everyone, if not for subsidies like this and the agribusiness CEOs, their lobbyists and the politicians making the subsidies happen.
Is it a coincidence that one of the top sources of calories in the United States, high-fructose corn syrup (HFCS), is made from one of the most heavily subsidized crops — corn?
I think not.
HFCS is in many processed food items you would never expect, including diet foods and “enhanced” water products. Even most infant formulas contain the sugar equivalent of one can of Coca-Cola! Government subsidies have also allowed corn to become a staple in animal feeds, which means even animal-based foods like conventionally-raised meats are tainted or nutritionally altered by HFCS.
Recently, some companies have begun to replace HFCS with regular beet sugar in a few of their products as more and more people learn about HFCS and protest against it, but still, one of the effects of the farm bill is to create a negative feedback loop that perpetuates the highly profitable standard American diet.
These junk-food subsidies make it much cheaper to buy a burger, fries, and soda from a fast-food restaurant than it is to buy grass-fed beef and veggies. It's not that these natural and organic foods necessarily cost more to grow or produce; it’s just that the prices for the junk foods are being artificially reduced by the government.
The end result is a food culture that is a primary driver of diabetes and disease, rather than a primary driver of health!
According to one meta-analysis, drinking just ONE soda — or other sweetened drink, including sweetened, bottled water with vitamins in it — per day can raise your risk of developing diabetes by 25 percent, compared to drinking just one sugary drink per month.
Diabetes Drugs Are NOT the Answer
The failure of conventional medicine to effectively prevent and treat diabetes is most evident in the dangerous drugs it promotes, foremost of which is Avandia. Avandia hit the market in 1999, after the mounting of a multimillion-dollar ad campaign that made it a blockbuster drug. By 2006, Avandia’s annual revenue was 3.2 billion dollars.
Avandia sales, however, plummeted to 1.2 billion dollars in 2009, two years after a study published in the New England Journal of Medicine5 linked Avandia to a 43 percent increased risk of heart attack, along with a 64 percent higher risk of cardiovascular death (compared to patients treated with other methods).
In the end, more than 50,000 lawsuits were filed against Avandia’s maker, GlaxoSmithKline (GSK), after it became public that as many as 100,000 heart attacks could be blamed on this drug.6 GSK settled the lawsuits in 2013 by agreeing to pay in excess of $229 million — but only to “avoid the expense and uncertainty of protracted litigation and trial,” a GSK spokesperson said, while at the same time denying any wrong-doing on the part of the drug company.
You would have thought that the FDA’s next move would have been to order this drug off the market.
But in a show of either bias or callousness, a committee of independent experts recommended that Avandia remain on the market despite the risks. An FDA oversight board voted 8 to 7 to accept the advice.
Avandia works by making diabetes patients more sensitive to their own insulin in order to control blood sugar levels. It specifically reduces your blood sugar by raising the sensitivity of your liver, fat, and muscle cells to insulin.
In fact, most conventional type 2 diabetes treatments use drugs that either raise insulin or lower blood sugar.
As I have already explained, the problem is that diabetes is NOT a disease of blood sugar. Focusing on the symptom of diabetes (which is elevated blood sugar) rather than addressing the root cause is an exercise in futility and could even be downright dangerous. Nearly 100 percent of type 2 diabetics can be successfully cured without drugs. You just might be surprised to know that you can eat, exercise, and live your way to recovery.
Effective Diabetes Diet and Lifestyle Tips
I’ve simplified the various effective ways to increase your insulin and leptin sensitivity – and to prevent or reverse diabetes – into six easy, highly doable steps.
- Exercise. Contrary to prevailing recommendations of shunning exercise during illness, staying fit is highly important in getting diabetes and other diseases under control. In fact, it is one of the fastest, most powerful ways to lower your insulin and leptin resistance. Get a head start today by reading more about Peak Fitness and high-intensity interval training – less workout time, more benefits.
- Eliminate grains and sugars and ALL processed foods, especially those made with fructose and HFCS. Conventional diabetes treatment has failed over the last 50 years partly because of its seriously flawed dietary principles.
Eliminate ALL sugars and grains – even “healthful” ones like whole, organic, or sprouted grains – from your diet. Avoid breads, pasta, cereals, rice, potatoes, and corn (which is, in fact, a grain). Until your blood sugar gets under control, you may want to restrict fruits as well.
It’s particularly important to eliminate processed meats. In a groundbreaking study comparing processed meats to unprocessed meats for the first time,7,8 researchers at Harvard School of Public Health found that eating processed meat is associated with a 42 percent higher risk of heart disease and a 19 percent higher risk of type 2 diabetes. Interestingly, they did not find any risk of heart disease or diabetes among individuals eating unprocessed red meat such as beef, pork, or lamb.
- Besides fructose, eliminate trans fats, which increase your risk for diabetes and inflammation by interfering with your insulin receptors.9
- Get plenty of omega-3 fats from a high-quality, animal-based source.
- Monitor your fasting insulin level. Every bit as important as your fasting blood sugar, your fasting insulin level, or A1-C, should be between 2 and 4. The higher your level, the worse your insulin sensitivity is.
- Get probiotics. Your gut is a living ecosystem of a multitude of bacteria. The more good bacteria you have, the stronger your immunity and the better your overall function will be. Optimize your gut flora by consuming fermented foods like natto, miso, kefir, raw organic cheese, and cultured vegetables. You may also take a high-quality probiotic supplement.
How Sun Exposure Can Help Treat and Prevent Diabetes
Have you been getting adequate sun exposure?
Hundreds of studies are now confirming the power of vitamin D, a steroid hormone, to influence virtually every cell in your body. Receptors that respond to vitamin D have been found in nearly every type of human cell, from your bones to your brain.
Recent research shows that women can help reduce their children’s risk of type 1 diabetes by optimizing their vitamin D levels prior to and during pregnancy, as vitamin D has been shown to suppress certain cells of the immune system that may be a factor in the disease.
And, new evidence strongly supports that vitamin D is highly beneficial not only in juvenile type 1 diabetes,10 but also in type 2 diabetes.11,12
Other studies published between 1990 and 200913 also revealed a significant link between high levels of vitamin D and a lowered risk of developing type 2 diabetes, along with cardiovascular disease and metabolic syndrome. It will likely take decades before health policy catches up with what overwhelming scientific evidence has already revealed about the benefits of vitamin D, and before increased sunlight exposure becomes the norm. But you don’t have to take part in the waiting game – you can optimize your levels right NOW.
Ideally, you should regularly expose a large amount of your skin to healthy amounts of sunshine, preferably as close to solar noon as possible. Direct UV exposure translates to up to 20,000 units of vitamin D a day. You may also use a safe tanning bed or supplement with oral vitamin D3. If you choose to do the latter, have your vitamin D levels routinely tested by a proficient lab to see if you are within the therapeutic range. Follow age-appropriate vitamin D doses when supplementing.
| VITAMIN D DOSE RECOMMENDATIONS | |
| AGE | DOSAGE |
| Below 5 | 35 units per pound per day |
| Age 5 to 10 | 2500 units |
| Age 18 to 30 | 8000 units |
| Pregnant Women | 8000 units |
WARNING:
The ONLY way to know whether the above recommendations will
help you achieve your optimal D levels is to test your blood. You
might need 4 to5 times the amount recommended above, or you might need
less. Ideally your blood level of 25(OH)D should be 60ng/ml. |
|
Don't Be a Diabetes Statistic – Take Control of Your Health
To summarize:
- Type 2 diabetes is a fully preventable, reversible condition that arises from faulty leptin signaling and insulin resistance. It is possible to control or reverse your diabetes without drugs by recovering your insulin and leptin sensitivities. The only known way to reestablish proper leptin and insulin signaling is through a proper diet and exercise. There is NO drug that can currently accomplish this, and I doubt if one will ever exist in the lifetime of anyone reading this!
- A meta-analysis of 13 randomized controlled trials involving more than 33,000 people showed that drug treatment of type 2 diabetes is not only ineffective, it's dangerous. Treatment with glucose-lowering drugs actually showed the potential to increase your risk of death from heart-related and all other causes.
So please remember, your diet will make or break you if you're diabetic or pre-diabetic. Unfortunately, the conventional dietary recommendations for diabetics – that of a high complex carbohydrate, low saturated fat diet – is the exact opposite of what actually works.
High complex carbohydrates include legumes, potatoes, corn, rice, and grain products. Aside from legumes, you actually want to AVOID all the rest to prevent insulin resistance. Nearly all type 2 diabetics need to swap out their grains and sugars for other foods, such as protein, green veggies, and healthy sources of fat.
- You will want to take special care to eliminate from your diet fructose and high-fructose corn syrup, which is far more detrimental than any other type of sugar. Drinking just one sweetened drink a day can raise your diabetes risk by 25 percent compared to drinking one sugary drink per month, so you really need to evaluate your diet and look for hidden sources of sugar and fructose.
This also means avoiding most processed foods of all kinds, as they are loaded with fructose. You especially need to avoid processed meats which, along with added sodium, have sugar in them to make them palatable.
You may also even need to avoid fruits until your blood sugar is under control.
I strongly advise keeping your total fructose consumption below 25 grams per day. However, it would be wise for most people to limit fructose to 15 grams or less, as it is virtually guaranteed you will be getting "hidden" sources of fructose from just about any processed food you eat.
Following my nutrition plan will help you do this without much fuss, as it walks you through the steps you need to get back on the road to optimal health.
The good news is that you don’t have to be a part of the diabetes epidemic. To avoid becoming a dismal statistic, you merely need to make some lifestyle changes and be mindful about your habits from day to day. In fact, just resolving to be healthier14,15 may reduce your risk for diabetes!
As I explain in my new book, Effortless Healing: 9 Simple Ways to Sidestep Illness, Shed Excess Weight, and Help Your Body Fix Itself, your healing plan is in your hands.
References:
- 1 CDC. Prediabetes: Could It Be You. CDC National Diabetes Statistics Report. 2014, Online. (Accessed December 2014)
- 2 Lipman TH, et al. Increasing Incidence of Type 1 Diabetes in Youth. Diabetes Care. June 2013. Online. (Accessed January 2015)
- 3 Mercola.com. Clinical Scientist Sets the Record Straight on Hazards of Sugar. January 5, 2014.
- 4 Rogers D. Bigger Subsidies Under New Farm Bill Program. Politico. March 9, 2015. Online. (Accessed September 2015)
- 5Nissan SE, et al. Effect of Rosiglitazone on the Risk of Myocardial Infarction and Death from Cardiovascular Causes. New England Journal of Medicine. June 2007. Online. (Accessed September 2015)
- 6 Drug Watch. Avandia Heart Attack & Congestive Heart Failure. Drugwatch.com. June 16, 2014. Online. (Accessed September 2015)
- 7 Micha R, et al. Red and Processed Meat Consumption and Risk of Incident Coronary Heart Disease, Stroke, and Diabetes Mellitus. Circulation. May 17, 2010. Online. (Accessed February 2015)
- 8 Harvard School of Public Health. Eating Processed Meats, but not Unprocessed Red Meats, May Raise Risk of Heart Disease and Diabetes. Harvard News. May 17, 2010. Online. (Accessed February 2015)
- 9 Angelieri CT, et al. Trans Fatty Acid Intake Is Associated with Insulin Sensitivity but Independently of Inflammation. Brazilian Journal of Medical and Biological Research. July 2012. Online. (Accessed February 2015)
- 10 Aljabri KS. Glycemic Changes after Vitamin D Supplementation in Patients with Type 1 Diabetes Mellitus and Vitamin D Deficiency. Annals of Saudi Medicine. Nov-Dec 2010. Online. (Accessed February 2015)
- 11 Herrman M, et al. Serum 25-Hydroxy Vitamin D: A Predictor of Macrovascular and Microvascular Complications in Patients with Type 2 Diabetes. Diabetes Care. December 18, 2014. Online.(Accessed February 2015)
- 12 Dalgard C, et al. Vitamin D Status in Relation to Glucose Metabolism and Type 2 Diabetes in Septuagenarians. Diabetes Care. June 2011. Online. (Accessed February 2015)
- 13 Parker J, Hashmi O, Dutton D, et al. Levels of Vitamin D and Cardiometablic Disorders: Systematic Review and Meta-Analysis. Maturitas. March 2010. Online.(Accessed September 2015)
- 14 Long GH, et al. Healthy Behaviours and 10-Year Incidence of Diabetes: A Population Cohort Study. Preventive Medicine. February 2015. Online. (Accessed February 2015)
- 15 Hackethal V. Resolve to Be Healthier May Actually Help Reduce T2DM. Consultant Live. December 30, 2014. Online. (Accessed February 2015)
No comments:
Post a Comment